With all of the health issues brought on by the COVID-19 pandemic, LIMRA research shows employees are placing greater importance on the benefits offered by their employers, and are more closely examining their benefit needs.
In 2020, LIMRA asked full-time employees with insurance benefits what changes they made to their benefits package during their 2020 open enrollment period. The results highlight the immediate short-term impact of the pandemic.
Last year, 3 in 10 full-time employees made a change to their benefits selections — the majority (8 in 10) adding or increasing coverages. For those employees who made changes to their benefits selections, 2 in 10 indicated the pandemic was one of several reasons behind the changes they made; only 2% stated that COVID-19 alone drove their benefit decisions.The top three benefits that were added/increased were life insurance, medical insurance, and dental insurance.
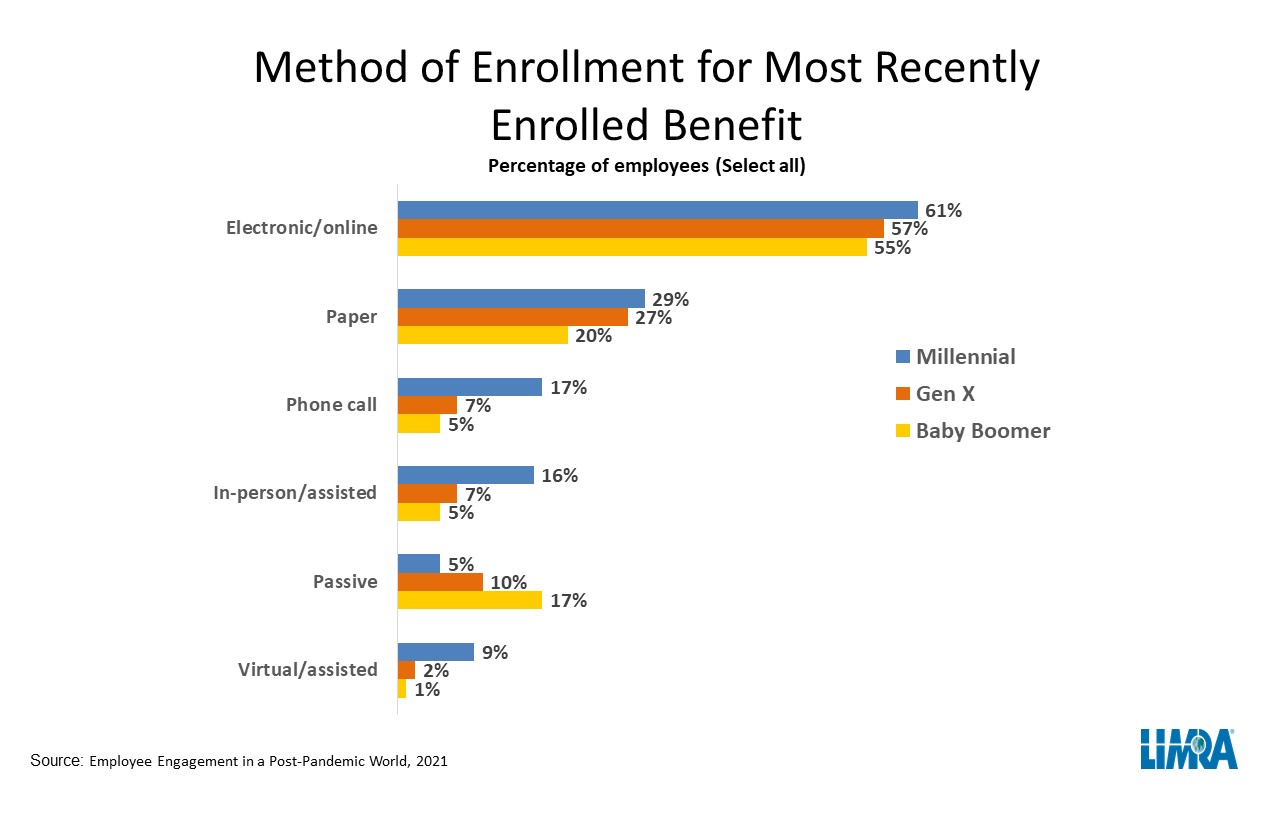
When it comes to how employees enrolled in benefits, other LIMRA research shows nearly 6 in 10 employees recently enrolled in their benefits online, through the internet or company intranet. Paper is the next most common method at 27%.
Employees at large employers (1,000 or more employees) are more likely than those at small employers (fewer than 100 employees) to enroll electronically/online (69% and 40%, respectively).
The research also looked at how employees choose to engage with their benefits carriers. The most common reason employees engage their benefits provider is because they are looking for information about the benefit in general (32%) or what is specifically covered (31%).
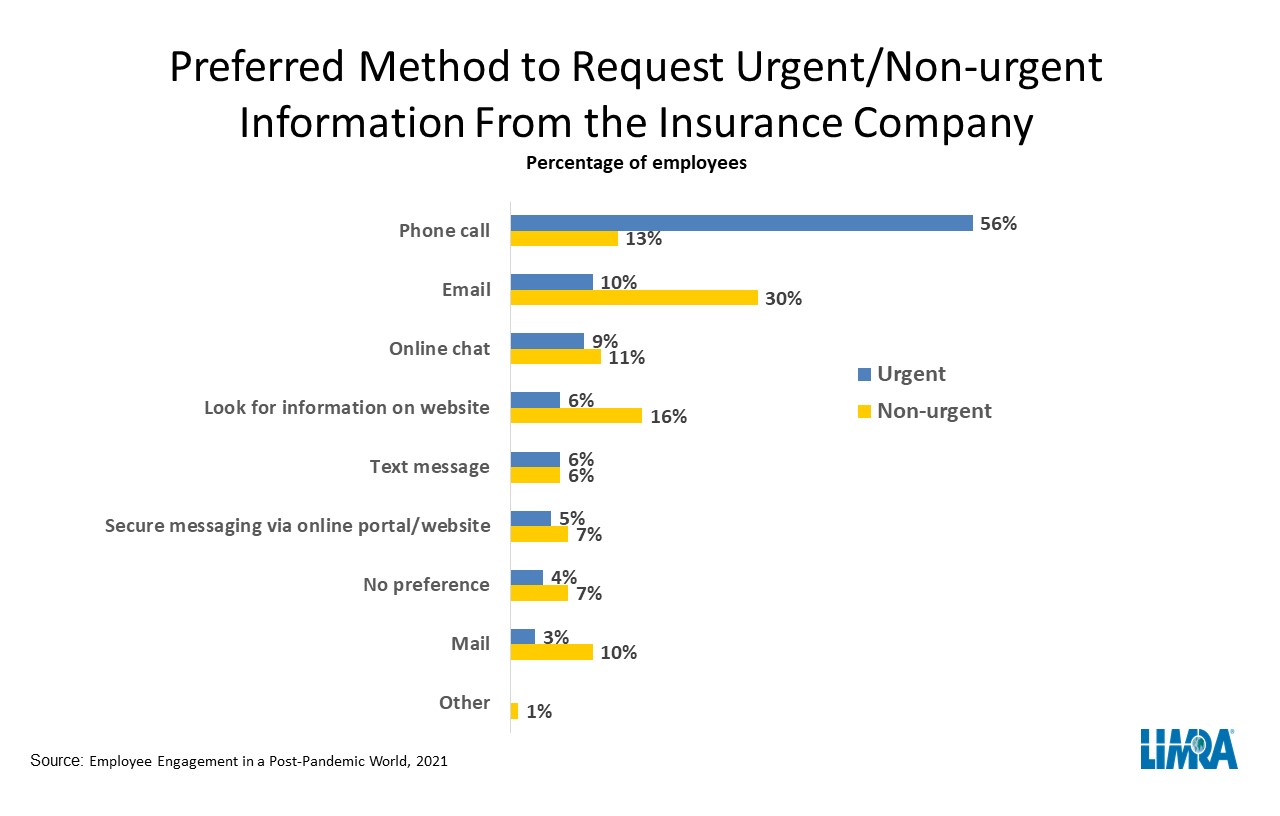
The study finds most employees (70%) prefer to engage with their benefits provider digitally (email, texting, online chat, etc.) for non-urgent issues. However, if the issue is urgent, the majority (56%) want to call their provider.
“The workplace benefits marketplace continues to evolve,” says Mary Lesch, associate research director, Workplace Benefits Research, LIMRA. “Companies that can appreciate the nuances of employee engagement preferences and align their engagement methods accordingly will be well-positioned to connect employees with the coverages they need and deliver a positive employee experience.”
This article is provided by NAIFA partner LIMRA. For members, you can learn more about LIMRA and how to partner within the Member Portal.